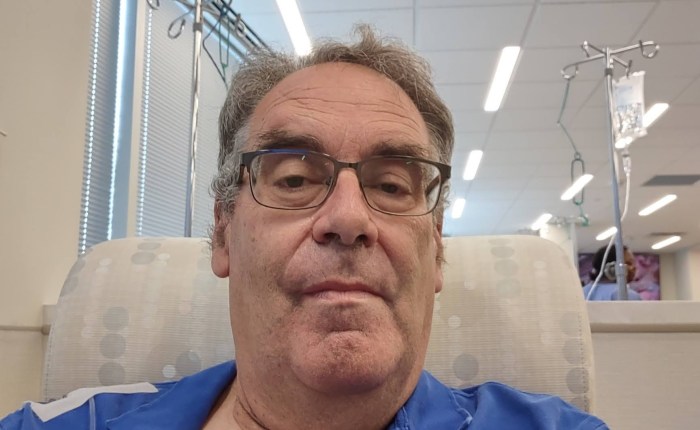
What I am posting today was written at the beginning of my Chemo treatments. Tomorrow (February 14th) will mark treatment #10 of 12 as well as Valentine’s Day, Ash Wednesday, and my 70th Birthday. As I prepare this particular chapter, the thought hit me; if we knew what the future held when we started on a particular journey, would we still go through with it?
Food for thought.
By the way, there are two chapters this week.
The First Cycle
October 9th through the 13th included appointments with three different doctors (or nurse practitioners), the infusion, two sets of labs and a return visit to return a pump I would get on Wednesday (10/11).
My first Monday visit was with my Oncologist’s nurse practitioner. I saw it as sort of a final “Pep Rally” for what was to come. I still had lots of questions needing to be answered. Carol was with me on this visit so that she might answer questions that I may not have even thought of. Having a nurse as a wife comes in handy from time to time. This time, knowing that I had an opportunity to ask more questions, I prepared ahead, writing questions on note cards, making certain that I had the right questions I needed to ask.
That session went extremely well. I appreciate the fact that my questions were answered in a straightforward manner.
The second medical encounter was with Texas Vision and Lazer Center. I had been with them for several years due to a referral from my optician. There was concern that because my Maternal Grandmother had Glaucoma in the last part of her life, I might be subject to the same disease. On an earlier visit, TVLC determined that I was developing Cataracts, so, we’ve been keeping tabs on the Cataracts.
There was a gap between my visit to Texas Oncology and TVLC which we used to do a little restocking with Costco and to grab a sandwich. Costco was easy. Grabbing the sandwich was a little trickier. We only had so much time between Costco and my appointment with TVLC. The sandwich shop we decided on was a bit slower than it could have been, causing me to have to boot having to eat the sandwich until later.
My sandwich (a Wagyu Beef Sub) was well worth the wait and was good for two meals.
TVLC was only doing some preliminary testing which lasted no more than fifteen minutes. Another visit was scheduled for the following Monday.
My visit with My PCP allowed me enough time to go home, pet Filbrix, eat half of my sandwich, and a leisurely drive over the river and through the woods to the good doctor’s office.
“You won’t believe what’s happened since the last time I saw you.”
It had been three months since I had seen my PCP, and a week and a half until a scheduled “Wellness Visit” as part of Medicare. He was unaware of my failed Trifecta in July, my diagnosis, the operation, and the port. We concentrated on my right leg and what needed to be done so I could walk normally. (The crutches and the wheelchair had been retired by the time of this visit.)
After the business with the leg, he and I talked about my upcoming Chemotherapy session. He assured me that I had the right Oncologist for the job (he once had an office near my Oncologist) and that he stated (tongue firmly in cheek) the best thing about her is that she was one of very few people shorter than he is.
I reminded him of our upcoming Well Visit and the labs he ordered on the 12th. After pondering a moment, he and I agreed that blood work done on the 12th would be rather useless since I would be pumping chemicals into my veins. That would throw the whole purpose of getting blood work in the first place.
All the ducks were in a row for Wednesday and Friday. Except one.
There was a deductible involved.
I got the call on Tuesday afternoon and was given a figure that would have caused trouble had I not been prudent with the household finances over the previous several months. Being operated on and then having to go through Chemotherapy ain’t cheap.
Wednesday morning. I had been bracing for Wednesday morning for the better part of a month – not knowing what to expect, despite having been briefed on what would come to be when I got there.
I took two bags with me containing what I thought I might need for my first infusion session. As a precaution, I arranged for rides to and from the center. Before my ride arrived, I showered, shaved, and before getting dressed, applied a Lidocaine ointment on top of the skin on top of the port. Lidocaine is a topical anesthetic used to keep the insertion of a needle into the port from causing me discomfort. To keep the Lidocaine in place, I had a clear bandage covering the port site provided from a stock Carol had in reserve.
The ducks were in a row.
My ride to the infusion center came almost precisely at the time he needed to be there, getting me to the infusion center with no problems. My driver had a few stories about his encounters with cancer, including an ongoing struggle with prostate cancer, and pointing out where a niece of his would be opening a restaurant after the first of the year in a block of buildings under construction.
I walked into the infusion center filled with apprehension of what would happen to me that morning and in the next couple of days.
Fortunately there were lots of friendly faces to greet me every step of the way with the process.
The Process
To be clear, the infusion center is integral with the Oncologist’s office which is integral with Baylor Scott White – McKinney.
When I arrived at the infusion center, I was already familiar with at least some of the office layout and was prepared to an extent as to what would happen.
After getting checked in and making the four-figure deductible payment, it was hurry up and wait for blood work, followed by hurry up and wait to go into the infusion center proper.
What I found out later in the process was the blood work needed to be analyzed to prepare the proper doses of the medicines I needed. While I was sitting in a waiting room for my turn to come, my Oncologist and a Pharmacist were determining what medicines I needed, in what dose.
After attempting to read for a while, I finally decided that if I were to start going through my Facebook feed, I would be called in and at least that part of the wait would be over. It worked. After only five minutes with my phone, I was called back to the infusion room.
It started with the usual – blood pressure, heart rate, oxygenation, weight. Preliminaries done; I was shown to a chair in a section of the room where no one else had yet settled. I was given a short orientation of what would be happening to me over the next few hours. I was also given a binder telling me about my treatment, the medicines I would be getting (and the possible side effects of taking those medicines), and resources I could refer to if I had questions not covered by the binder.
The preliminary medicines arrived, and it was time to connect to the port.
Prior to heading to my infusion center, I was instructed to put on a quantity of numbing cream over the port, over which I put a clear bandage. My job at the center was to expose the port while the nurse removed the bandage. After a quick clean of the area, a needle was inserted into the port.
OUCH!
First lesson learned. Use more of the numbing cream before heading to the infusion session. The poke wasn’t that bad. It was bearable and the pain was extremely short lived.
I finally settled in with my feet up and ready to roll. I read a little bit (starting to re-read Tolkein’s Lord of the Rings series of books) before I found another inmate, rather a pair of inmates settling on the opposite side of the section where I was sitting.
Through conversation, I learned that both were veterans – one Vietnam era, the other during Desert Storm. Both had experience overseas. The Vietnam Vet told stories of clandestine activities he had been aware of while he was there. I heard some of those stories before, passed along by a long-time friend who was part of the Vietnam experience. The Desert Storm Vet was quiet about his experiences. He spent most of his time in Germany, as did another long-time friend of mine who had a similar experience.
Both men were seasoned veterans of another sort; both had had several Chemotherapy treatments before this round; both were treated for lung cancer. The Vietnam Vet told of his first time around with Chemo when he was in a group of several other men. According to him, the other men in his group gave up after four or five treatments… those who quit died within three months of quitting treatment. Not something I wanted to hear while I was being infused for the first time. I still had aftereffects to deal with.
The most immediate aftereffect I had to deal with was using the bathroom. I tended to forget that I was being pumped full of liquids and that at some point, I needed to empty my bladder. The problem I had was that I was hooked to a machine that was plugged into the wall behind me. I finally worked up the courage to ask the nurse to unhook the apparatus from the wall so I could pilot the stand and myself to one of the two restrooms.
I waited too long.
No, I made it to the toilet with no leakage, but my prostrate was irritated by some of the drugs I had been given to the point that I had very little flow trickling down from a very full (and no doubt a very irritated) bladder.
Lesson learned; don’t wait too long to use the bathroom while being infused… and drink something else to make things easier on the prostate and the bladder